This blog post article aims to cover an overview of the most eventful years of concierge medicine and how it has cemented itself as a major player in the present healthcare landscape.
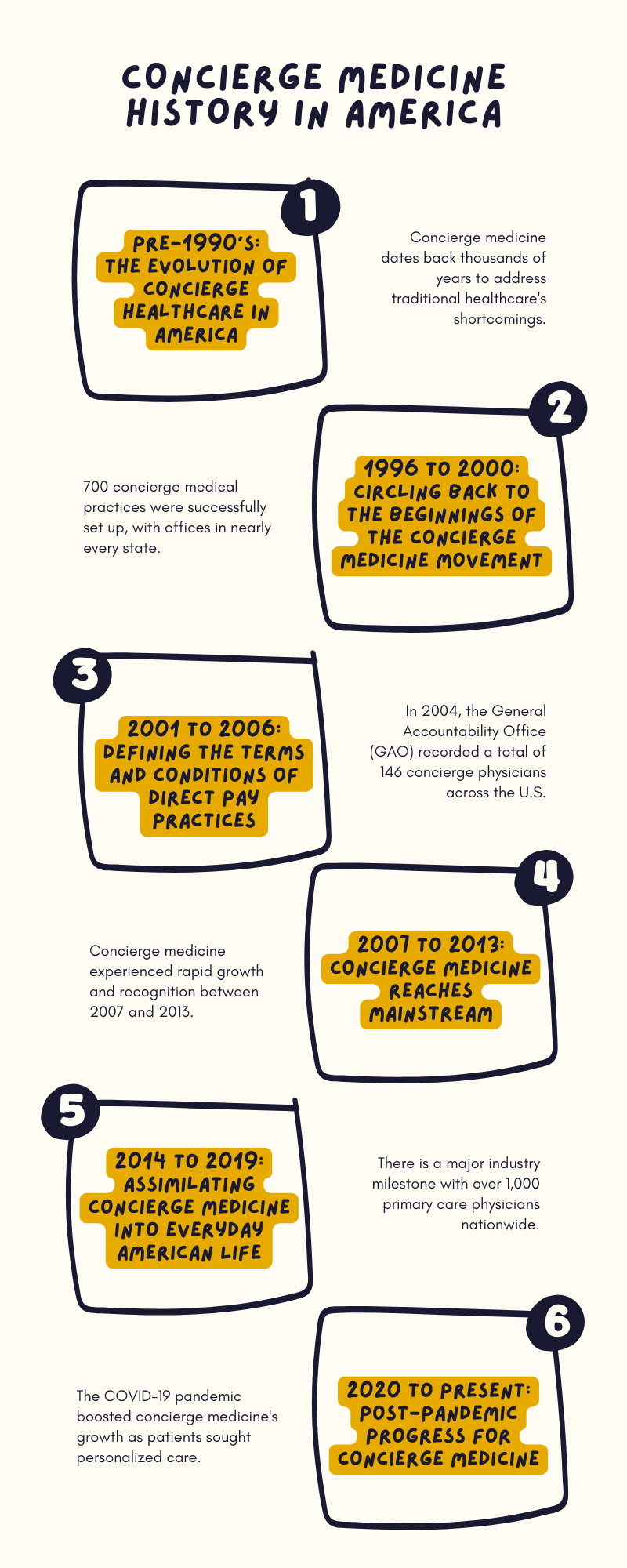
The idea of a direct relationship between doctors and their patients existed well before the term ‘concierge medicine’ was coined. It served as the cornerstone of healthcare / standard healthcare practice in America, and across the world, for thousands of years.
Prior to the insurance-based model, patients would pay doctors directly (with no help from intermediaries), and the healthcare extended was more personalized and holistic.
The origins of health insurance plans date back to the mid 19th century. By the time the 1980’s rolled around, the concept of healthcare insurance gained traction and eventually grew into today’s traditional, insurance-dominant healthcare industry.
At the time, it seemed like a great option for patients until the healthcare industry started focusing more on their profitability and less on what mattered most: patient-centered care.
This flawed system led to doctors being overworked and out of touch with their patients. It resulted in poor health outcomes, high healthcare costs, and an estranged relationship between doctor and patient.
This fall-out led to the rebirth of the healthcare industry in the late 1990’s. Direct patient care, also known as ‘concierge medicine’, was born.
The earliest iteration of concierge medicine began in 1996. Dr. Howard Maron and Scott Hall, FACP set up a direct pay practice in Seattle, Bellevue, WA and Oregon, charging an annual retainer fee of $13,200 and $20,000 for every family they would see.
This is recognized in concierge healthcare history as the first form of a direct pay practice offered to patients in the U.S.
In 1999, representatives from the American College of Physicians (ACP) and the American Board of Internal Medicine drafted a charter that would serve as a framework of how professionalism can be implemented in direct pay practices.
That same year, the Institute of Medicine released a medical report concierge medicine physicians would refer to for medical errors, patient safety, and professional integrity.
The earliest recorded medical center who first offered concierge medicine services was Virginia Mason Medical Center in Seattle, WA during the year 2000.
Later that year, Dr. Robert Colton and Bernard Kaminetsky, set up MDVIP in Boca Raton, FL.
MDVIP is a concierge medicine practice and medical management firm which successfully set up more than 700 concierge medical practices with offices in almost every State.
The American Medical Association (AMA) published the official concierge medicine physician guidelines called the ‘Principles of Medical Ethics’ in 2001.
In the same year, retainer medicine took root in Seattle in the form of MD2 (pronounced as “MD squared”). Dr. Howard Maron, former team doctor of the Seattle SuperSonics, together with his partner Dr. Scott Hall, began a peaceful revolution in healthcare.
Duane Dobrowits, chief executive officer of MD2, described their undertaking as ‘the Ritz Carlton of medical care’.
For the first time, healthcare centers had marble-lined bathrooms; fine art hung on the walls; and doctors saw patients one at a time to uphold privacy, as well as to enforce that personal doctor-patient relationship.
Lower cost / more affordable versions, such as Seattle Medical Associates and the Lewis & John Dare Center at Virginia Mason Medical Center, have since emerged.
These concierge medicine collectives and direct pay practices regularly onboard physicians to meet patient demand, with hundreds of patients being on the waitlist.
In 2002, Medicare addressed concierge medicine and its retainer fees. In a memorandum by the Centers for Medicare and Medicaid (CMS), the group expressed their position on concierge medicine.
They stated that physicians were free to enter into retainer medicine set-ups, for as long as they do not violate any Medicare requirements.
By 2003, Dr. John Blanchard founded the American Society of Concierge Physicians, which was later on re-named to Society for Innovative Practice Design (SIMPD).
Concierge medicine practices were also ruled as not illegal by the Department of Health and Human Services. Consequently, the federal government and the Office of the Inspector General (OIG), took a hands-off approach on concierge medicine.
The AMA Council on Ethical and Judicial Affairs set guidelines for “contracted medical services” in June 2003. The AMA House of Delegates later on approved these guidelines for industry use.
In 2004, the General Accountability Office (GAO) recorded a total of 146 concierge physicians across the U.S. Later that year, a study by Harvard University revealed that 55% of its respondents were dissatisfied with the traditional healthcare they receive, and 40% of that 55% agreed that the quality of care had worsened in the last five years.
A study conducted by MDVIP in 2006, reported that 130 doctors within their concierge medicine network treat up to 40,000 patients all over the world.
In 2007, the first concierge media publication went live. Concierge Medicine Today was created as an advocate and central hub of news regarding anything related to concierge and retainer practices and the direct care industry.
2007 was also the year wherein the term “direct practice” was first used in legislation in Washington.
During said legislative session, they clarified that direct care practices were not affiliated with insurance companies under state law, but they also offered basic medical care to patients.
By 2008, Orange County, CA clocked in 35 concierge physician practices within their district alone, putting them on the map as a leading hub of concierge medicine.
Private medicine history also witnessed significant industry developments between 2008 to 2009. These include the formation of non-profit organizations, as well as analytics and research collectives.
In 2010, SIMPD rebranded itself as the American Academy of Private Physicians (AAPP) and expanded its reach via their first local chapter in Orange County, CA.
There was a rise in media publications and research collectives within the concierge medicine space during this period.
Concierge Medicine Today reported the increasing affordability of concierge medicine practices across the U.S., with 62% of the programs costing less than $135 per month.
By the end of 2012, MDVIP also released a report showing that there had been a dramatic reduction in hospitalizations as well as $300 worth of monthly savings because of their personalized concierge medicine models.
New data in 2013 also showed there was higher career satisfaction among concierge medicine and direct primary care (DPC) physicians. That same year, the AAFP recognized the value of concierge and direct pay practices within family medicine and created a universal DPC policy.
In addition, Concierge Medicine Today detailed the distinction between a concierge medicine subscription versus health insurance.
They explained that because concierge medicine is not insurance (i.e., it would not cover a trip to the hospital), a retainer medicine subscription works best with a high-deductible plan.
“Think of health insurance more like auto insurance or fire insurance; it should be used for emergencies. Your concierge medicine subscription, on the other hand, should cover the day-to-day.”
On October 11-12, 2013, the very first DPC National Summit was held.
Dr. Erika Bliss, president and CEO of Qliance Medical Management Inc., expressed during the momentous event, “DPC is quickly becoming an important contributor to the transformation of our nation’s healthcare system.”
The first DPC National Summit also awakened the fact that direct pay practices were thriving at this point in personalized medicine history.
There were four states that were considered as leading players in active concierge practices as well as high patient interest: Florida, California, Pennsylvania and Virginia.
In each of these states, there was a significant number of people seeking out concierge physicians and cash-only options.
In April 2014, Comstock’s Magazine compared the difference in cost between traditional healthcare and concierge medicine.
They indicated that the average cost of traditional healthcare insurance premiums in America is $328 per month, in contrast to $150 a month for concierge fees plus bare-bone premiums for a high-deductible plan that cost around $110.
In September 2014, the American Academy of Private Physicians (AAPP) cited that the industry is focused on five key areas.
These five areas are: “legal compliance for doctors, innovative learning tracks at national meetings, physician networking, legislative and lobbying initiatives and staying up to date on new and emerging technologies”.
The industry witnessed a dip in the concierge medicine timeline between 2015 to 2017. A handful of practices closed down, including a few notable ones like Qliance and Turntable Health.
This has led the government to set up a bill requiring the Office of the Insurance Commissioner (OIC) to furnish annual reports to the Legislature regarding direct healthcare practices.
RCW 48.150.100(3) details that these reports include, but are not limited to, “participation trends, complaints received, voluntary data reported by the direct practices and any necessary modifications to this chapter.”
The board of directors of the AAPP voted to put operations on hold and to re-evaluate the association’s value proposition in August 2017. The association issued a statement following their cease in operations.
“Due to evolving marketplace conditions in the private medicine conference space, our AAPP board of directors voted to suspend operations in 2017 and to re-evaluate AAPP’s ongoing usefulness and value proposition for 2018 and beyond.”
In 2018 and 2019, online resources and forums on concierge medicine flourished and multiplied in number. During this period, MDVIP also reported a major industry milestone of more than 1,000 primary care physicians nationwide.
Concierge transition expert Specialdocs reported rapid growth within its network of independent concierge medicine practices in the wake of the COVID-19 pandemic.
As per Specialdocs CEO Terry Bauer, "During the COVID-19 crisis, it became clearer than ever that our concierge medicine model provides a proven, sustainable path to stability and success for independent physicians."
At a time when human interactions were restricted and limited, the appeal of direct, personalized care from a trusted physician rose to an all-time high.
Case in point, Northern Virginia, Atlanta and San Diego-based concierge medicine practices that launched right before the pandemic reported steady growth during this otherwise tumultuous time.
The COVID-19 pandemic was a key period in the evolution of concierge medicine because the perceived value of direct pay practices was unprecedented at this point in time.
Patients increasingly craved for the peace of mind that is rooted from knowing your physician was directly and continuously available anytime you needed them.
A survey conducted in 2021 among 3,500 respondents showed a zero percent pandemic closure rate for membership-based practices. These concierge medicine practices were even optimistic for the post-pandemic years that were to come.
The entire healthcare industry underwent a major pressure test during the COVID-19 pandemic, and concierge medicine is set to soar even higher 2024 onwards.
As we officially put the pandemic behind us, it is evident that healthcare cannot return to its status quo. Terry Bauer, CEO of Specialdocs, puts the current state of concierge medicine into perspective.
“Every aspect of our system has been tested to the extreme [during the pandemic], resulting in the core values of concierge medicine – personalized, preventive, long-term, patient-centered care – resonating as never before.”
The concierge medicine landscape has gone through significant updates within the last few years.
The IRS has laid down the groundwork in terms of how concierge medicine subscriptions integrate with a Health Savings Account (HSA) or Flexible Spending Account (FSA).
Having regulatory clarity is a revolutionary step in extending more health care options to patients and allowing them to receive the quality of care they deserve.
As per current IRS regulations, patients are now allowed to use their HSA or FSA accounts to pay the monthly retainer fee for concierge medicine.
That being said, most medical services accumulated within a patient’s concierge membership are eligible for reimbursement. These include prescriptions, laboratory examinations, co-pays, annual physicals/visits and other out-of-pocket expenses.
For all accumulated medical expenses, keeping sufficient documentation is important when it comes to filing reimbursements / using FSA/HSA.
As for advanced physical work-ups and plan restrictions, it is best to confirm with your provider which expenses are eligible for reimbursement.
Read more about: Is the Membership Fee for Concierge Medicine a Tax Deductible?
Concierge medicine collectives like the DPC Coalition and Health Rosetta have been at the forefront of healthcare reform.
The industry has witnessed major developments in technological integration, policy influence, financial inclusions in HSAs and FSAs, broader adaptation of concierge medicine and the public health sector as a whole.
These organizations have rendered important work to put value-based and patient care-focused healthcare on the radar of federal and state legislation.
Concierge medicine is currently undergoing major legislative developments, as two bipartisan bills are moving through Congress.
These two bills are H.R. 3029 (The Primary Care Enhancement Act) and H.R. 3836 (The Medicaid Primary Care Improvement Act), with the latter already passed by the U.S. House of Representatives this 2024.
Both bipartisan bills are designed to expand DPC access to both private and Medicaid patients.
H.R. 3029, or the Primary Care Enhancement Act, is great news for patients who have HSAs and HDHPs. Once passed, H.R. 3029 would allow patients to use HSA accounts to pay for DPC fees.
As of November 2024, the bipartisan bill is currently awaiting the approval of the full House of Representatives. The bill has already made its way through the House Ways and Means Committee, as it is included in a larger bill, H.R. 5688.
If H.R. 3029 is passed, Americans across the country can finally reap the benefits of concierge medicine, using the pre-tax dollars from their HSAs.
Next, congratulations are in order as H.R. 3836, also known as The Medicaid Primary Care Improvement Act, was passed during the latter part of 2024.
The bill indicates that Medicaid programs can offer direct primary care services without patients having to secure a federal waiver from the Centers for Medicare & Medicaid Services (CMS).
Thanks to Reps. Dan Crenshaw (R-TX) and Kim Schrier, MD (D-WA) for championing the bill, H.R. 3836 was passed with unanimous support (28-0) and is now awaiting further implementation from the House.
H.R. 3836 simplifies DPC for Medicaid patients, by doing away with the complicated and lengthy process of having to secure a waiver from CMS.
This will spearhead DPC accessibility across more states, giving low-income patients the opportunity to experience the value of having a DPC or concierge medicine arrangement at their disposal.
In terms of DPC legislation on an industry-wide scale, federal regulation encompasses Medicare and opt-out issues. These rules apply across the country. Consequently, all DPC practices are also required to comply with relevant federal healthcare laws.
Medicaid regulations and dispensing laws, on the other hand, are state-specific.
Many states implement Direct care-specific regulation that protects concierge medicine practices from being regarded and governed as insurance. You may refer to DPC Frontier’s state regulation guide here.
Movement in regulatory clarity is a telling implication that concierge medicine has indeed hit mainstream. At the time of writing this article, legislative bills are already in the pipeline concerning the inclusion of concierge medicine membership fees to be eligible for HSA and FSA reimbursement.
With doctors and patients in the concierge medicine space growing in number, the call for physician and patient protection has never been greater.
Federal and state regulation streamlines how concierge practices are run across the U.S., offering organized and coherent implementation to this highly promising healthcare model.